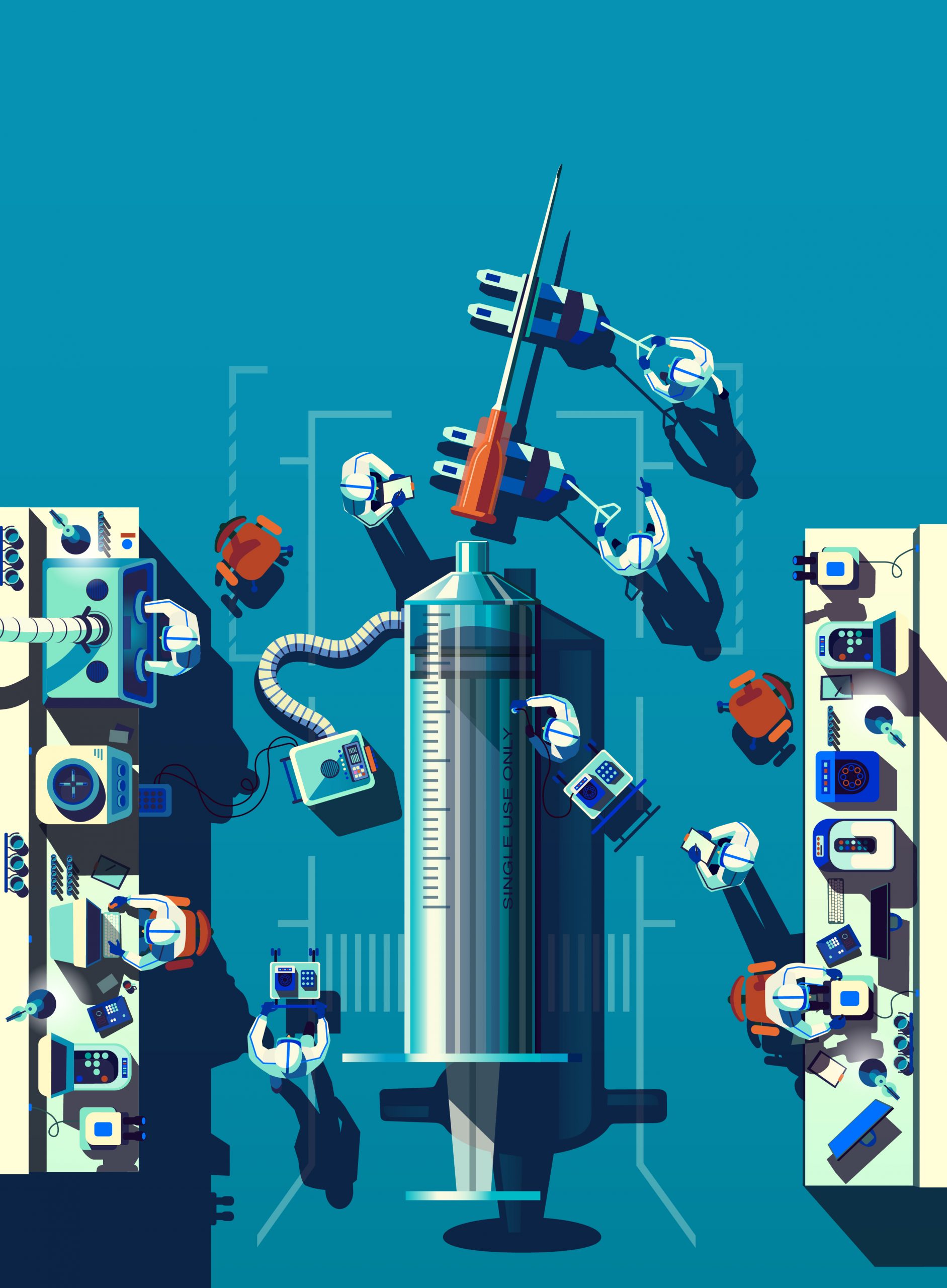
The smarter enemies thrive on surprise attacks. Virus and crown in particular are well aware. remain hidden in animal hosts for decades, sometimes mutate constantly, casually infectious agents into effective and efficient morphing. If a strain with the right combination of genetic code that spell trouble for people does the animal from jumping man, the ambush began. This was the case of SARS-CoV-2, the crown behind COVID-19, and the attack was mostly silent and insidious in the first. Many people infected with SARS-CoV-2 were blind, because they served as the virus of the new home and allows you to establish a foothold in the global human population. These hosts were the perfect base camp for the beginning of the attack, social, political policies, economic and inverted systems worldwide. The best hope for this attack when comparison is a vaccine research efforts underway furious effective blows ensue if the manufacturer is able to distribute enough people, and when people actually get enough of these immunized. The vaccines are based on the concept of herd immunity, a type of biological fortress, where the vast majority of the population protected from infection. A road has been infected by natural infection, which is enough for man and is recovering without serious consequences. But many public health experts say, forcing shops and schools open, people are so healthy that could not become seriously ill if infected develop immunity can be a dangerous strategy that leaves too much to chance; there is no way to predict how long it will take and continue on the road of harmful viruses and people who kill, become immune to enough people. The vaccines were the benefits of protection, without the pain and unpredictability-by Edward Jenner in 1790 discovered the scientific detour around natural immunity guarantees that expose people to low levels of the smallpox virus might give immunity the disease. Today, pharmaceutical and biotechnology companies to develop, or more than 100 COVID-19 vaccine candidates and billions of dollars governments trial in a massive global effort pumps as we have seen since the polio epidemic of the 1950s Everything about this vaccine could take the story makes the speed to be developed with the recordings, how they have been tested and authorized as they handed people around the world. first identified by scientists month the new crown, the Chinese team to test already nearly 10 potential vaccines. Powered by President Donald Trump speed of bending operation that will provide at least $10 billion in promised federal funding for research and COVID-19 candidate vaccine trial is the United States is performed three late-stage studies in healthy volunteers. Other countries, including Italy, Russia, Japan, Singapore, South Korea, Australia and India have created all human testing of its vaccine for life. The warp speed operation promises an ambitious 300 million doses of January 2021 to provide; have to do so, manufacturers including Moderna, AstraZeneca, Pfizer, Sanofi and Johnson & Johnson already started their candidates produced vaccines ongoing studies show that they are effective. Ei US Centers for Disease Control and Prevention warned governors in early September the government plan Diseases (CDC) as the initial dose can be ordered and delivered when available. These are all calculated risks, the most full of tensions between the development policy needs and to restart economies educational institutions and the needs of rigorous scientific and regulatory process that sent a data threshold showing that a new vaccine is safe and effective before it can be released to the public. Russia had announced in August that its Ministry of Health, a vaccine by the Moscow scientists developed approved, which was still being tested was considered premature by the scientific community and potentially dangerous strongly criticized for the high-risk groups who would receive the first . In September, shortly after the major vaccine manufacturers in an unusual show of solidarity, committed to achieving security full studies on their vaccinations before they were submitted for regulatory review, set Zeneca his ice study, so the researchers an unexplained illness in one of the study participants to investigate. These actions serve as a reminder that the development and testing of these vaccines is already loaded to the yield point. Headquartered in Massachusetts Moderna Therapeutics, together with scientists from the National Institute of Allergy and Infectious Diseases of the government (NIAID), already recorded prepares a candidate for human trials by developing and in 42 days, a process that has taken in recent years . And it is why the accelerated schedule to come up with a dose of humility. to develop the search for a vaccine for a new infectious disease is a gamble at best; nearly four decades after HIV was discovered, there is still no effective vaccine against the virus. SARS-CoV-2 is so new in the scientific community that there is not even clear what the needs of the human body to prevent infection, or if such a thing even possible. The urgency of the pandemic means doctors have only worth a month of information from studies of how long it might take the immunity of the shots. As some experts, including those to develop the vaccine, saying they should expect at best a vaccine that the effects of the disease to minimize, rather than the offer of “sterilizing immunity”, people would completely protect against ‘ infection. “For many respiratory pathogens, it is a challenge to get an immune response sterilization,” says Dr. Evan Anderson, associate professor of medicine at Emory University School of Medicine and lead researcher on one of the modern studies. “We do not know if this is the case of SARS-CoV-2”. Another challenge: Only one likely will not be enough vaccine. From the point of view of production and distribution, population immunization different vaccines in the world and probably takes the contribution of all companies currently pushing for the production of a product. “This is a global problem, and no company is the solution”, says John Shiver, senior vice president of vaccine research around the world and development at Sanofi, a French pharmaceutical company. “Because we do not know what works, what works best, or what best serve the need for really, really stop the pandemic, more shots on goal are important.” Even with different vaccines, will not be easy, its the right people at the right time to arrive for sure. Almost all candidates will need two shots, until a month or so away separately. Some vaccines must be maintained at temperatures below the freezing point of the production plant to close when they are injected into the arm of a person. And if vaccines are delivered to hospitals and clinics, which should be immunized before? The most aggressive production plans are not yet sufficient to vaccinate all vaccines, mainly produce in the first few months. Health experts have to make about how to deploy the first precious cans and turn on ethical principles such as risk of difficult decisions and social benefits. This put healthcare workers, people with existing health conditions and the elderly in residential facilities of the group towards the top of the list, as well as first responders and other key professions such as teachers, law enforcement and management of waste. But, notes Dr. Ezekiel Emanuel, Vice Provost for Global Initiatives at the University of Pennsylvania, these discussions did not address the practicality. Up to 40% of the health conditions of the existing US population would qualify them likely to be available for priority vaccination far more than the number of doses that will be the first production runs. “We never thought through, because it is a difficult problem and therefore we avoided,” he says. As some of the most promising racing vaccines through the final stages of testing, however, can not be avoided, and decisions about global lottery must be made of this precious resource decisions that the difference between such a pandemic could mean his death and continue tragic attack on human life and slows down at the end. How to decide who is first obtained a crown vaccine in general the most part, the issue of distribution, the number of vaccine must receive begins each country. Any benefit from the hope of herd immunity given by the vaccines fades, if not enough of the population of the “flock” of the world-is immunized and protected against infection. Researchers at the CUNY Graduate School of Public Health and health policy used to calculate a computer simulation that, if 75% of the world population has been immunized, vaccines would be effective for the protection against infection by 70%, to control the current pandemic. If only 60% were vaccinated, then the threshold of effectiveness would jump to 80%. And a safe and effective batch of vaccine production, even from deep pharmaceutical company experience with a track record of millions of doses of other vaccines, it is not a slam dunk. “In making vaccines, is the research, development, implementation, then,” says Dr. Paul Offit, chief of the Vaccine Education Center is used hospital of Philadelphia’s children, in the US American Food and Drug Administration (FDA) Committee to advise the Agency COVID-19 vaccine approvals director. “The most difficult of these three is the implementation. Mass production is not trivial; made perfect condition, and you learn as you go.” During the campaign of US polio vaccination in 1950, he notes, a manufacturer could properly the polio virus in the vaccines used to inactivate and 40,000 children were infected. to achieve the challenges of such widespread vaccination, not only to achieve production goals. Dozens of countries are investing to develop their own vaccines or, and there are nationalist arguments to convey the final products of these investments to those who remained, which funds, the country would close out with fewer resources for the health of the cans they need . Even in industrialized countries, are able to produce enough vaccines, recording may be difficult, as anti-vaccine mood in general (largely stems from unfounded links between certain vaccines and autism) and concern for the safety of any COVID- 19 vaccines, in particular, in a recent survey conducted by the World Economic Forum Ipsos commissioned a third of Americans said they would not be vaccinated if a 19-COVID is shot available. A certain amount of nationalism from the perspective of social justice makes sense, says Emanuel, anywhere in a global health crisis, allowing the virus to infiltrate anywhere is a threat to people. For the need for international unity to mark the World Health Organization with the vaccine-focused alliance between public and private Gavi together and the Coalition for innovations Epidemic Preparedness, a group of philanthropists and governments focused resources required to meet the threats of diseases infectious expected to COVAX-forming device, a mechanism which nations would buy vaccines reduced price to enable pooling their purchasing power. The initiative helps fund can sign nine vaccine candidates, and countries to make commitments to buy the shots effectively terminate at volume discounts. So far, 172 countries have expressed interest in participating, including 80 industrialized countries and 92 lower and middle income countries. The Trump administration refused COVAX citing ongoing tensions with WHO, but even without the United States, COVAX now represents 70% of the population of the world to join. International experts have proposed two major strategies to decide how much get-one vaccine that countries should one country and the other is based on the population, the share of health workers is used as a guide, one of which fall short Emanuel believes sufficient distribution. “People want to be ethics, but do not know what it is ethical in this context,” he says. In his view, these are principles to reduce damage, premature death and economic difficulties and limit the spread of the community of diseases that would bring more people in danger. Even when countries get their assigned dose, to decide what people should first raises more ethical and practical challenges are immunized. In the US National Academies of Sciences, Engineering and Medicine published a draft of the priority guidelines in September suggests four levels of vaccination groups. The first wave of vaccinations for high-risk groups, including health professionals, people with existing medical conditions such as obesity, asthma and heart disease and the elderly in the group conditions of life would be. The following are the workers “critical risk”, teachers, the elderly, people in homes and imprisoned; then young adults and children; and finally the rest of the nation. A final project reflects public comments on these proposals is responsible for the vaccination recommendations for COVID-19 vaccines to be attributed to the CDC Committee. While waiting, Dr. Nancy Messonnier, director of the National Center for Immunization and Respiratory Diseases at the CDC, has informed early August, health authorities in four states (North Dakota, Florida, California and Minnesota) and city (Philadelphia) that would be part of a pilot program to roll out vaccines, CDC and operating at warp speed would gather data from pilot sites to refine plans for vaccines to the rest of the country are assigned. “Our goal,” said CDC Director Dr. Robert Redfield in August “is no delay in the handover between the FDA to ensure a national level of immunization and vaccination programs for approval.” All this obviously depends on the fact that tens of thousands of volunteers COVID-19 vaccine candidates in recent studies to develop strong immune responses to obtain SARS-CoV-2 without serious side effects. As innovation accelerates the process of COVID-19 vaccine development Carol Kelly, associate director of nutrition at Emory University Student Health, an application for its Next Door application in April saw volunteers in a study near a COVID-19 vaccine Search for participating candidates, he was immediately fascinated. He called and found out that this particular study could test a vaccine based on a new genetic technology. No vaccine using this technology was approved, although a handful of diseases such as respiratory syncytial virus and influenza, is in evidence. “They said that contains the genetic code of the virus. This type of data has made me think,” says Kelly. But they signed anyway. “I felt powerless to see me, who work so hard in the health sector … I thought, it’s a little ‘what I can do to further develop a solution to run and help, why not?” The Emory study testing a vaccine jointly by scientists from NIAID and Modern. If successful, it could be a new type of vaccines that would be agitated in the history of pioneering the fastest. Some existing vaccines, including flu shots for producers to grow to cause disease over a period of weeks, large amounts of viruses or bacteria, then turn off in the lab, not the can, but they are still quite unknown to alert and activate the defenses of the human immune system to mount against them. One of the main reasons Modern has been able to move so quickly that bypasses this process and relies instead on the mRNA, the genetic material for proteins. On 10 January, Chinese scientists published the first complete genome sequence of SARS-CoV-2; after only 42 days had the Modern NIAID team used that code to identify which parts would viral genome good targets for the development of a vaccine specific for the protein Spike, the code that SARS-CoV-2 defined. It surrounds the outer shell of the virus like a crown, the spike protein also serves as Lockpicker to break in healthy human cells. Once inside, the SARS-CoV 2 hijacking those cells of the pump outside the machine more copies of itself throughout the body and spread continue to infect its mission and replication. The way Dr. Stephen Hoge, President of the Modern, it seems, “mRNA is really like a software molecule in biology. So our vaccine as the software program for the body, which then goes and makes proteins viral [] to generate an immune response. “Modern manufactured and shipped its first vial of vaccine for human trials by the end of February, three months later, he had his first batch of data from a few healthy volunteers in a small studio in the early stage. The vaccine appeared immune safe and seemed Veran antibodies against SARS-CoV-2 in similar quantities to produce in people who had recovered from COVID-19 Kelly kept a diary of their temperature and unusual symptoms for seven days after the first shot, saying that did not affect her very much, and the research team took blood samples every week until his second shot about three weeks later. The injection has met tougher; “Oh my heck, it was the next day I ran out,” he says. “I was just blown away, I had a bit ‘of dizziness and headache, and I never headache. I also had a little’ fever. But the next day I was fine.” Kelly takes her symptoms as a sign that the vaccine has done its job and that their immune system is to defend the company against SARS-CoV-2 triggered. Data from a subset of volunteers in the first phase of the studies seem to support that: new antibodies, which was formed to have to neutralize after vaccination appeared laboratory versions made from SARS-CoV-2. Inspired by these early studies, Modern begun a study in June to determine the ideal dosage and at the end of July, launched the final phase of testing, which will include 30,000 volunteers who received either dose or a placebo. The speed with which Modern was to develop capable and start the test was a tempting lesson during other developers of vaccines. Leading professionals in the pharmaceutical industry have begun mRNA their priority programs in technology with smaller biotech companies with expertise had developed. For example, Pfizer, the pharmaceutical giant based in New York, a collaboration of two years with German companies took advantage of immunotherapy Biontech and April paid $185 million in a joint effort four potential vaccines based on mRNA to explore. The two companies had been working to create mRNA for the use of a vaccine against influenza, and if COVID-19 hit, says Philip Dormitzer, Vice President and Chief Scientific Officer for Viral Vaccines to Pfizer, “it was relatively easy to swap the ‘encoding influenza antigens put in the candidate vaccines and antigens in COVID-19 in place of “Such substitutions are one of the strongest features of the mRNA technology. however a lot of live virus is required, all the researchers is to find the correct code, the genetic sequence of the virus, which then modified antigens to the immune system to make the intrusion virus alert. Pfizer and Biontech scientists exploited this and quickly developed four promising candidates for the examination; Early studies identified the entire genetic sequence of the virus spike protein comprises how to generate the side effects associated with fewer robust immune response. In late July, the company began a phase 2 and phase 3 of the combined process of this candidate with 30,000 people. Pfizer is not the only company betting accelerated in mRNA technology. In June, Sanofi raised its stake in Trans Bio, which could amount to $1.9 billion and give Sanofi access to technology and production know-how based mRNA vaccines against infectious diseases develop with-COVID-19 the obvious priority. The companies are working to start clinical trials in humans sometime this year. But while manufacturers of mRNA vaccine platform can provide a jump-start in development, Family vaccine approaches have a well-established production and storage methods behind them. For one thing, the mRNA is notoriously unstable and sensitive to temperature, so as to do with this need vaccine technology are anywhere from -94 ° F (-70 ° C) at -4 ° stored and shipped away under F (-20 ° C), the temperatures for the majority of existing vaccines. Therefore, companies such as Sanofi, Johnson & Johnson and AstraZeneca are innovative on their experiences with others, but promising process of production of the vaccine, citing to solve this problem-one, which is a different virus. Since viruses are sent to infect cells, they may be the immune cells of the body until a useful vehicle for the transport of other viruses to trigger, as they are initially disabled. Pharmaceutical companies build and testing of vaccines against Ebola, influenza and RSV, including Trojan-horsing genetic material of a virus inside the shell of another that does not cause disease in the position, but questions remain about as safe as double-virus vaccines could be. A Johnson & Johnson, based in New Brunswick, NJ, include scientists in weakened form of adenovirus, which is responsible for the common cold, to provide COVID-19 material. His hopes of the team that shot, unlike many of the other candidates COVID-19 vaccine will only need one dose. The company plans to start from September, both single and double doses to test his vaccine. In the UK, scientists at Oxford University are using a similar approach to their vaccine is developed, manufactured and marketed by AstraZeneca. They added the genetic code for SARS-CoV spike protein-2 in a cold carrier weakened virus, which usually infects chimpanzees. The cold virus transported the viral genetic material from human cells and “infected” to it would be in the same manner SARS-CoV-2, and then the immune system prepares a natural infection works the same way to attack. In early human studies, the vaccine has produced good immune responses to SARS-CoV-2. The Oxford-Zeneca team believes that its manufacturing process for this kind of shot to make it easier manufacturing, scale-up. “Hopefully, if it is successful, the vaccine will be relatively inexpensive to make in dollars per dose, and is relatively easy to do on a large scale,” Mene Pangalos, executive vice president says the research and development biopharmaceutical Zeneca. There may be a price for the ease of production, however: focusing on vectors like that can lead to common cold problems down the road. First, exposure to two viruses, even if one is weakened, an excessive immune response that could trigger more ends to cause inflammation that could be useful harmful. Second, while the cold virus are first sent to the cells to infect the human immune system is also adept at learning their dissipation. So while a base of cold virus vaccine may be an immune response against SARS-CoV-2 to the initial production, to be effective if a person is exposed once again, that the immune response may not be as robust second time. This is a real concern for public health, as most officials are on a wave of new cases in autumn and winter, when flu cases also voltage spikes. The study, which expanded by AstraZeneca 50,000 people in the US, UK, Brazil and South Africa is currently suspended as researchers are investigating whether a disease that is experienced by the study volunteers together on the vaccine. The unexplained illness has been reported as part of routine security through surveillance of independent peer review process conducted by each vaccine are important process to ensure that new vaccines do not hurt cause more harm than good. Based on previous successful vaccine In a sense, the break is used in the study can also serve as evidence of the value of the proven strategies in attacking that have a wealth of success. Researchers also know from experience that a different approach based on genes, one that is based on the DNA, not only produces antibodies to a virus such as cells and B cells SARS-CoV-2, but also T that help the body a hard create more reminders from previous infections and better prepared to recognize and target viruses and bacteria should invade again. While antibodies against SARS-CoV-2 proteins are probably an important role in the final alchemy his immunity, there is evidence recovered from COVID-19 patients that these antibodies may not always be sufficient. Recent plasma analysis convalescent recovered COVID-19 patients in New York, for example, shows that antibody levels are very different and that most of these antibodies have only moderate forces SARS-CoV-2, at least to neutralize the lab. In addition, some studies suggest that the antibody level may disappear as soon as three months after infection. For durability and permanent protection against future infections, the body needs help to win his cell-mediated immune response, including T and B cells that have the ability to remember to recognize and reactivate against former enemies. While Modern reported that its vaccine good for mRNA T cell responses generated by DNA-based vaccines against other diseases have already demonstrated posted to this work. In part, this is what Sanofi-COVID 19 shot went through the partnership with GlaxoSmithKline (GSK) for another potential called a vaccine based on recombinant proteins. The approach involves the protein peak and, in the case of GSK and Sanofi have inserted in insect cells with the genetic code for parts of SARS-CoV-2 to produce the then serve as the factory of the viral protein. The researchers then extract and purify this protein and requires you to create defenses with a GSK link connection that, once injected, the human immune system, specifically antibodies against it. It is a reliable technique, and is responsible for HPV and hepatitis B vaccines, which were approved respectively in 2006 and the 1986th E ‘even technology that make Sanofi Flublok applications, its vaccine against influenza , which means that if his COVID-19 vaccine is safe and effective with this method produced, the production of the company was too fast. The company has begun human trials in September and a year earlier a billion doses provides when their effective vaccine. Australian scientists at Novavax also use an insect cell-based system to provide the genetic code of the SARS-CoV protein spike 2 as a vaccine, and the results reported in September encouraging. Meanwhile, in Inovio, based in Pennsylvania, researchers have conducted studies on experimental vaccine primates based on DNA for MERS use, and the results indicate that the animals were strong T cell responses in a better position, the MERS for neutralize the virus. “I think the level of T cell response will be very important in security features [against SARS-CoV-2],” says Dr. J. Joseph Kim, President and CEO of Inovio. The company has vaccinated the first 40 volunteers in a clinical trial phase 1 for its COVID-19 vaccine in April and reported in June, without going into details, deeper that 94% of participants has produced a immune response. Inovio also consider designing its vaccine in the case. The next step: Production and sales Although vaccine manufacturers can be found in the newly viral spark right to catalyze an immune response against SARS-CoV-2, are facing another equally difficult task: making enough of these vaccines in the shortest possible time to throw the brakes on runaway pandemic. Zeneca CEO has committed to produce 2 billion doses of vaccine by the end of the year an ambitious timetable. But local experts cautious note that there is a chance, however remote, that the tests in the course of the vaccines have demonstrated the dramatic effectiveness and stopped soon, later this year. If this is possible is to a large extent depend on the diffusion-19 COVID is reached when many of the final stages of testing vaccines. These studies are more focused on action than on safety and require tens of thousands of participants. If there are not enough cases of COVID-19 still in the latter test does not start the statistical power they need in order to compare with the exposed virus to those people who have been a vaccinated with recipients in circulating placebo scientists time and see rapidly if the vaccine works. Such was the fate of SARS and MERS governments immunization programs and drug between 2003 and 2012 launched every company. Once the cases have decreased, it has the urgent need for vaccines and, together with investments in research and experimentation. Some public health experts believe that if this work had continued what researchers have learned the crown would be and how to protect against it has given scientists a jump start for a vaccine against SARS-CoV-2. To avoid losing the momentum once again, some epidemiologists have the idea of intentionally infecting volunteers for COVID-19 floated vaccine trials. Known as “Man Challenge” Research is a questionable strategy and it was done only with diseases such as flu and malaria, is that people can take to make them difficult, exposed to ill after intentionally to disease for net treatments good safety when receiving. For now are the ethical questions this approach raises no urgent, as new hot spots continue to appear around the world. The biggest and most immediate problem when vaccines were approved, it’s like they do for people who need it most. In the United States already in the public health systems are overwhelmed by cases of testing and monitoring the pandemic and the urgent care needs, “yesterday”, according to one of the officials of the state as health plan for a massive vaccination campaign, how many doses can to expect and how they decide who gets those first doses. “Our public health system is highly fragmented, under-resource, overlooked and undervalued,” says Dr. Howard Koh, professor at Harvard T.H. Chan School of Public Health and former Secretary of State for Health and Social Affairs. “To make this possible, the local public health infrastructure and state must be very strong, and it is not now.” The situation is similar disastrous in lower resource countries like India, where the shortage of hospital beds and medical equipment, the burden and the toll the disease is increased. Regardless of what vaccines are successful in clinical trials, the coverage will reach key herd immunity. A key coverage once provided access depends on the price. Modern said that its vaccine is priced according to the volume of ordered doses, with smaller volumes will cost a maximum of about $32 to $37 per dose, while AstraZeneca says his Oxford collaborative vaccine developed and deployed cost to meet the needs to meet in low -resource countries. for the production in advance of the final results of his studies, Zeneca signed agreements with companies in South Korea, Japan and Brazil and provide up to 3 billion doses of its vaccine. “It’s not going to win us and to lose someone else. The point is to make us the difference of this disease,” said Pangalos AstraZeneca. Although COVID-19 vaccines do not provide 100% protection against infection, which could provide a huge boost to this return to normal. But how quickly that happens on the science behind them so much it will depend on how humanity that determines where do these vaccines. What is tested is that new technologies and the latest virus control strategies in each grossed injection. ‘Also our desire to be blind to the physical and social and economic boundaries that separate us, to fight viruses that do not take these distortions. “With COVID-19 there is a chronic anxiety,” says Kelly. “To be relieved this is so important. It ‘s so important to have confidence that the vaccine to help us have a healthier society not based on fear, so that we again be able to enjoy our lives.” -With reporting by Ciara Nugent / London, Leslie Dickstein, Mariah Espada and Simmone Shah Copyright by Illustration by Peter Greenwood TIME
Related Post
More than half of Americans fear that the pressure of the White House for a coronavirus vaccine will Rushed
For weeks, the US president Donald Trump has repeatedly forecasts, sometimes bordering on promises that a COVID-19 vaccine is imminent. "We remain on track to...
COVID-19 is devastating even nursing homes. The administration Trump does not do much to stop it
At least 75,000 Americans in nursing homes and other structures have long-term care as soon as they died COVID-19 and the devastation is far from...
COVID-19 has killed nearly 200,000 Americans. How many more lives will be lost before the US makes it right?
Forty-five days before the announcement of the first suspected case of what the COVID-19 would be known, the global index of the Health Security has...
Zeneca has taken its COVID-19 vaccine trial after a break for the security check
This story has been updated to reflect AstraZeneca's investigational vaccine shot. AstraZeneca, the British pharmaceutical company behind one of the most promising candidates COVID-19 vaccine...
Nearly 2 million fewer US teens are vaping now than last year, the data show CDC
Nearly 2 million fewer US teens report on e-cigarettes in 2020 compared to 2019, according to new data from the US Centers for Disease Control...
Depression rose during the 19-COVID Pandemic, Study Says
As soon lockdowns crown entry into force in March, the discussion turned to mental health. And 'well-it documented that natural disasters, wars and other mass...