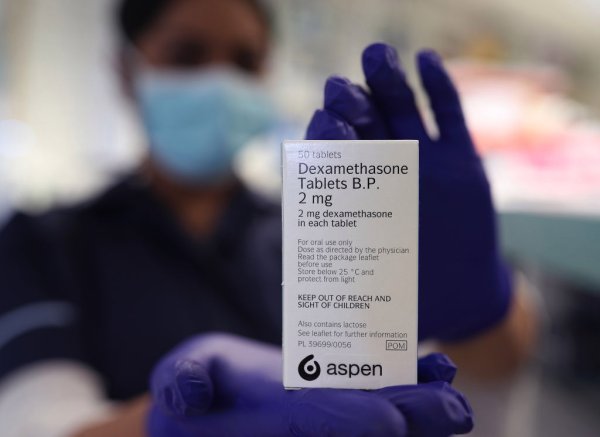
An article published Friday in the New England Journal of Medicine suggests that a low-cost steroid may be an effective treatment for severe COVID-19, based on encouraging preliminary results from last month. In June, British researchers reported that dexamethasone a cheap, widely used steroids, to reduce by one third the inflammation in the body appeared the risk of death in patients with severe to reduce COVID-19 operators have UK started dexamethasone on the same day the results were announced, but some medical experts were more guarded, to do with the topic, without any conclusion, the procedure should be made against the full results. These results were published today in the NEJM, and they seem to support what was announced last month. Dexamethasone has a measurable benefit to COVID-19 patients sick enough breath for the assistance, but there was no such benefit and also showed the potential for some possible harm to patients with mild disease. About 2,100 people hospitalized for confirmed or suspected COVID-19 were roughly a 10-day course of dexamethasone in addition to the standard 19-COVID care to be assigned, while 4,300 received standard therapy alone. Approximately 16% of patients (total, both those with dexamethasone and those who were not) received mechanical ventilation, 60% oxygen and 24% were receiving only received no help breathing. After 28 days, dexamethasone 482 patients who had died, compared to about 1,110 patients who did not. This means that about 23% of the dexamethasone-treated patients died, compared with about 26% of other patients. This may not seem like a terribly significant difference, but researchers have significant benefits for the most difficult patients affected in the sample: those who require mechanical ventilation to survive. About 30% of these patients died of dexamethasone compared to 41% of patients who do not. A smaller, but still significant benefit was observed for patients invasive ventilation oxygen. Meanwhile dexamethasone it provided no benefit for patients who are not breathing assistance was needed. In fact, in patients with these milder cases taking dexamethasone it was more need of-print% of them actually probably 18, compared with 14% of those treated with standard therapy alone. Logically, it seemed the anti-inflammatory drug used to work best in patients who have had the most inflammatory. He had developed on steroids as a patient in patients who have symptoms for at least a week and probably suffered with recent symptoms some inflammatory lung injury, it seemed better to make that much inflammation have not lived. “It ‘s likely that the positive effect of glucocorticoids that [dexamethasone] depends on selecting the right amount of serious respiratory viral infections, at the right time, in the right patient,” the researchers write in the paper. “Higher doses may be more harmful than useful, how can such confidential treatment in a time when viral replication is of utmost importance and inflammation is minimal.” While the publication of the newspaper is an encouraging step forward, if Provisional research to be confirmed by other researchers and replicated. The researchers also found that, because publish targeted results, in the shortest time possible to meet the demand for new treatments, they do not collect some data on secondary outcomes and long-term. Photo copyright Yui Mok / PA paintings- Getty Images
Related Post
COVID-19 is devastating even nursing homes. The administration Trump does not do much to stop it
At least 75,000 Americans in nursing homes and other structures have long-term care as soon as they died COVID-19 and the devastation is far from...
More than half of Americans fear that the pressure of the White House for a coronavirus vaccine will Rushed
For weeks, the US president Donald Trump has repeatedly forecasts, sometimes bordering on promises that a COVID-19 vaccine is imminent. "We remain on track to...
COVID-19 has killed nearly 200,000 Americans. How many more lives will be lost before the US makes it right?
Forty-five days before the announcement of the first suspected case of what the COVID-19 would be known, the global index of the Health Security has...
Zeneca has taken its COVID-19 vaccine trial after a break for the security check
This story has been updated to reflect AstraZeneca's investigational vaccine shot. AstraZeneca, the British pharmaceutical company behind one of the most promising candidates COVID-19 vaccine...
Nearly 2 million fewer US teens are vaping now than last year, the data show CDC
Nearly 2 million fewer US teens report on e-cigarettes in 2020 compared to 2019, according to new data from the US Centers for Disease Control...
The Great Race Vaccine: The unprecedented rush to immunize the world against COVID-19
The smarter enemies thrive on surprise attacks. Virus and crown in particular are well aware. remain hidden in animal hosts for decades, sometimes mutate constantly,...